Choosing the Ideal Endoscopic Enteral Access Method
At least 250,000 US hospitalized patients a year require enteral support using an artificial pathway into the gastrointestinal (GI) tract to deliver nutrition or medication. In light of this, the American Gastroenterological Association (AGA) has issued a Clinical Practice Update to improve the practice of endoscopic enteral access.
Covering indications, placement techniques, and management, the comprehensive document is a response to the increasing use of enteral access devices in chronic GI conditions. The update, published in Gastroenterology, addresses patient factors complicating placement decision-making such as thrombocytopenia, use of dual antiplatelet therapy, or performance of percutaneous access in the setting of cirrhosis.
“We provide clinical recommendations in these various scenarios understanding that the final decision-making is in the hands of the provider and care team,” said first author Dejan Micic, MD, a gastroenterologist and associate professor at University of Chicago Medical Center in Chicago at the time of the update (since relocated to Loyola University Medical Center in Chicago). “We hope this can serve a day-to-day purpose for clinical gastroenterologists and can be referenced as they encounter individuals with or needing an enteral access device.”
Traditionally, enteral access was reserved for patients with severe malnutrition or those unable to maintain oral intake. Recent recommendations emphasize early nutritional intervention including prehabilitation before major surgery, adjunctive therapy for oncology patients, and in specific inflammatory conditions such as Crohn’s disease. “These shifts recognize the role of enteral nutrition not only in preventing malnutrition but also as a therapeutic strategy,” Micic told Medscape Medical News.
There is, however, variability in the use of devices including the selection of appropriate units, technical aspects of placement, and subsequent management. “Such variability can lead to complications, suboptimal patient outcomes, and inefficiencies in care delivery,” Micic said.
He added that enteral access has been historically underemphasized in GI endoscopic training. “While procedural skill in placing devices such as percutaneous endoscopic gastrostomy, or PEG, tubes is often taught, a comprehensive understanding of the broader clinical context — such as proper patient selection, prevention of complications, and postplacement care — is not always thoroughly covered.”
The current update aims to bridge knowledge gaps with evidence-based-guidance. “It also underscores the importance of interdisciplinary collaboration with dietitians, nurses, and care givers to achieve the best outcomes for patients,” Micic said.
Commenting on the update but not involved with creating it, Shirley C. Paski, MD, MS, a gastroenterologist at the Cleveland Clinic in Cleveland, called it timely, adding, “As GI training is becoming more subspecialized and interventional radiology has been able to provide enteral access, gastroenterology training in enteral access has declined to where some fellows are graduating with limited enteral access experience.”
Yet malnutrition remains a common consequence when GI disease is severe, chronic, or refractory to treatment, or in the setting of postsurgical anatomy, she added. “Enteral nutrition is increasingly being considered a therapeutic or adjunct treatment in some cases of Crohn’s disease or small intestinal bacterial overgrowth. Gastroenterologists need the endoscopic skill to secure enteral access tubes, particularly in more challenging anatomy.”
Also commenting on the document but not involved in it, Steven Shamah, MD, director of Endoscopy at Northwell Lenox Hill Hospital in New York City, said, “This should serve as a concise review for any general hospitalist or gastroenterologist to understand what we have and when we should offer the proper feeding tube options.” He stressed, however, that all gastroenterologists should be trained in the placing of all of tube options.
“The axiom ‘If the gut works, we should use it’ is something that I was taught when I was a medical student and it still holds true,” Shamah continued. “There’s been a jump in interventional procedures to assure continuity of the GI tract even in progressive malignancy. So there’s a rise in moving away from intravenous nutrition and a rise in tube-delivered enteral nutrition.” Options for reducing reflux and aspiration will likely take on more importance, he said.
Tubing Options
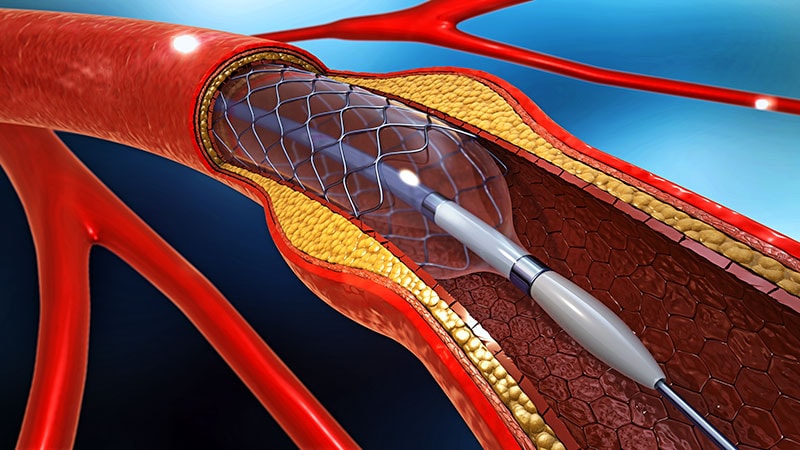
According to Micic and colleagues, recent data suggest a favorable safety profile of enteral feeding tubes placed endoscopically compared with surgical or radiologic placement. The illustrated AGA document outlines such approaches as synthetic flexible tubes placed into the stomach or small bowel via the oral (orogastric and oroenteral) or nasal routes (nasogastric [NG] and nasojejunal [NJ]) and percutaneous tubes accessing the stomach. The choice of tube, access point, delivery site, and feeding method varies with indication, expected duration of use, and patient anatomy, the authors stressed.
The update notes that NG and NJ tubes can be used immediately after confirmation of placement, most often with abdominal radiography. PEG tubes can be used immediately for medications and after 4 hours for tube feedings. A multidisciplinary team approach after placement provides improved patient care. “Dietitians assist with formula choice, volume, free water needs, and delivery method, and nurses and advanced practice clinicians assist with tube site assessment and troubleshooting.” the authors wrote.
Complications can occur but should be infrequent, Micic said. “Frankly, most complications can be predicted based on the duration of use and prevented with appropriate monitoring.” Common complications include tube dislodgement, clogging, site infections, buried bumper syndrome, and aspiration. “Minimizing these risks requires a thorough understanding of patient-specific factors, careful technique during placement, and ongoing monitoring after the device is in use,” he added.
Paski said the update aligns with established guidelines for enteral access but also offers suggestions to mitigate the risk of tube placement in patients in whom placement has traditionally been more challenging. “This is a helpful addition to the literature because if enteral access cannot be obtained in a patient unable to meet their needs orally, total paternal nutrition is the next and much more invasive step for nutrition support.”
She called the practice update a concise, comprehensive reference for trainees and experienced gastroenterologists to optimize placement conditions and reduce complication risk, noting that training in nutrition is suboptimal in many GI fellowships.
Becoming familiar with common and advanced enteral access techniques is within the armamentarium of all practicing gastroenterologists, the authors stated. Because malnutrition affects nearly all GI disorders, “Understanding common routes of enteral access and the basic principles of nutrition support promotes the initiation of optimal enteral nutrition, mitigating the impact of malnutrition, and improving prognosis for patients at nutritional risk,” they wrote.
Micic served on the advisory board for Ironwood Pharmaceuticals and is on the speaker’s bureau for Takeda Pharmaceuticals. Coauthor John Fang served as a consultant for Merit Medical, Circa Scientific, and Aspero Medical.
Paski and Shamah had disclosed no competing interests relevant to their comments.
Diana Swift is an independent medical journalist based in Toronto, Ontario, Canada.

 Admin_Adham
Admin_Adham