Which Ablative Therapies Are Best for Renal Cell Carcinoma?
For patients with primary localized renal cell carcinoma (RCC), especially those who aren’t good candidates for surgery, noninvasive or minimally invasive ablative treatments have emerged as important options. These ablative treatments include radiofrequency ablation (RFA), microwave ablation, cryoablation, and the relative new-comer stereotactic body radiotherapy (SBRT).
But how do these approaches stack up against each other?
A recent meta-analysis published in Lancet Oncology found that SBRT appears to be equally safe and potentially more effective than other ablative treatment options for localized RCC.
“Our findings suggest that SBRT might offer a particularly advantageous option for treating larger renal cell carcinoma tumors, yielding the highest local control rates among ablative options with comparatively low rates of severe complications,” Srinivas Raman, MD, Department of Radiation Oncology, Princess Margaret Cancer Centre, Toronto, Ontario, Canada, and colleagues wrote.
Outside experts who spoke with Medscape Medical News said SBRT should likely play a larger role in the management of early-stage RCC.
“Given its noninvasive nature, favorable toxicity profile, and comparable renal outcomes, SBRT warrants broader adoption,” said Shankar Siva, PhD, MBBS, a radiation oncologist at the Peter MacCallum Cancer Centre and professor at the University of Melbourne, both in Melbourne, Australia.
This new analysis is “helpful as it provides reassurance and further strong quality data to present in multidisciplinary renal rounds and tumor boards to consider the use of SBRT as an alternative to other ablative technique,” said Joelle Helou, MD, MSc, radiation oncologist, Verspeeten Family Cancer Centre, and assistant professor, Department of Oncology, Western University, both in London, Ontario, Canada.
Filling a Knowledge Gap
RCC is the most common malignancy of the kidney, accounting for > 90% of all renal malignancies. Worldwide, the incidence of RCC has continued to rise, with a 2% annual rate of increase over the past two decades.
The conventional treatment of choice is radical or partial nephrectomy; however, not all patients are ideally suited for surgery, especially those who are older or have compromised kidney function or comorbid conditions.
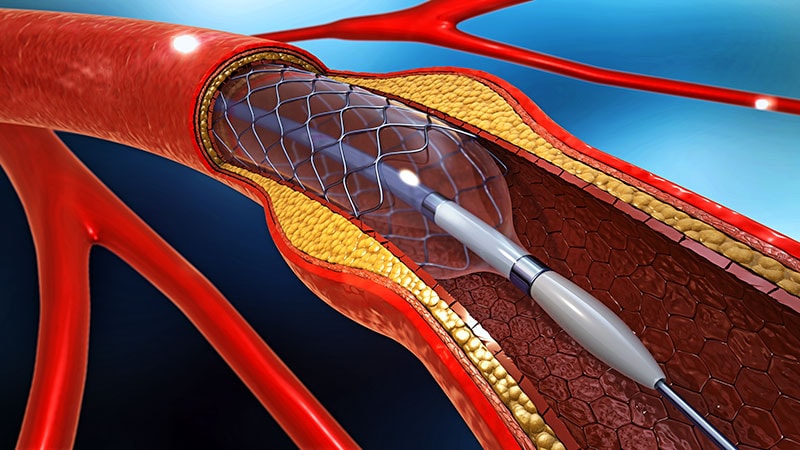
Ablative therapies have been integrated into clinical guidelines as evidence-based interventions to treat primary RCC. These therapies include RFA and microwave ablation — two minimally invasive thermal ablation techniques that use heat to destroy the tumor tissue — and cryoablation, which uses extreme cold to destroy the tumor tissue.
Studies have generally found similar outcomes with RFA and microwave ablation, with the choice of treatment often guided by what’s available and operator expertise. The US and European guidelines recommend these treatments, particularly for smaller tumors (< 4 cm), citing their effectiveness and minimal invasiveness.
SBRT is a relatively new noninvasive option that delivers highly focused radiation doses to the tumor across multiple sessions and may be particularly suited to larger tumors (≥ 4 cm).
National Comprehensive Cancer Network guidelines state that SBRT may be considered for nonoptimal surgical candidates with stage I, II, or III kidney cancer.
However, comparative data on these four techniques has been limited until now.
What Did the Meta-Analysis Find?
Raman and colleagues performed a systematic review and meta-analysis pooled data from 133 studies involving 8910 patients (mean age, 68 years) with localized RCC treated with one of the four ablative therapies.
Overall, across the four ablative approaches, local control rates were very similar at 1 year, ranging from 95% for cryoablation to 99% for SBRT, and at 2 years, ranging from 94% for cryoablation to 97% for SBRT. At 5 years, however, there was a slightly greater separation in outcomes favoring SBRT (95%) and RFA (92%) compared with cryoablation (90%) and microwave ablation (86%).
Although all four techniques demonstrated similar local control for small tumors measuring < 4 cm, the approaches began to diverge for larger tumors measuring ≥ 4 cm at 1, 2, and 5 years. At 5 years, for instance, SBRT had the highest local control rate (93%), outperforming RFA (79%), microwave ablation (82%), and cryoablation (85%).
Looking at survival outcomes, cancer-specific survival was 100% at 1 year across all treatments. At 5 years, small differences in cancer-specific survival were observed. For smaller tumors, cancer-specific survival ranged from 100% for both SBRT and RFA to 97% for microwave ablation and 98% for cryoablation. For larger tumors, the cancer-specific survival rate was 100% for microwave ablation, 95% for SBRT, and 94% for cryoablation.
These small differences in cancer-specific survival likely reflect differences in patient and tumor characteristics across the treatment groups, the study authors said.
Notably, patients treated with SBRT were older than those treated with microwave ablation and RFA, while also having the largest tumors, which have consistently been shown to be associated with worse local control, greater propensity for regional and distant metastases, worse survival outcomes, and increased treatment-related toxicity, the authors explained.
There were no significant differences in the rate of grade 1-2 adverse events between the ablative methods, although grade 3-4 adverse events occurred in a significantly higher proportion of patients treated with cryoablation (3%) than in those who received RFA and SBRT (2%) or microwave ablation (1%). Baseline or change in renal function, as measured by estimated glomerular filtration rate, did not differ between the ablative techniques.
Overall, the findings reinforce that, although typically offered to older patients with worse baseline renal function and much larger tumors, “SBRT maintained high effectiveness at 1, 2, and 5 years compared to thermal ablation,” Siva told Medscape Medical News.
SBRT in Clinical Practice?
Despite the mounting evidence in favor of SBRT for primary localized RCC unsuitable for surgery, “there is still some reluctance from urologists, mainly, to refer patients for consideration of SBRT,” Helou told Medscape Medical News.
This hesitance is reflected in the meta-analysis, he noted, with SBRT being the least performed ablative therapy (612 patients). Cryoablation was the most common technique used in 3726 patients, followed by RFA (2503 patients) and microwave ablation (2069 patients).
The “compelling efficacy and safety data suggest SBRT should play a larger role in managing early-stage RCC in nonsurgical candidates, particularly for larger tumors where it offers excellent long-term local control,” said Siva, who led the phase 2 FASTTRACK II study evaluating SBRT in patients with inoperable or high-risk primary RCC.
Despite patients having larger than average tumors (4.6 cm) compared with those in many other trials, Siva and colleagues reported a 100% local control rate following SBRT and no patient deaths from cancer during the study period
The FASTTRACK II study marked “an inflection point for SBRT, and [the approach] is now slowly getting traction,” Chad Tang, MD, radiation oncologist, MD Anderson Cancer Center, Houston, told Medscape Medical News.
Overall, Raman and colleagues said decisions about ablative therapy should be “precisely tailored to the individual patient’s clinical condition and treatment objectives.” Treatment selection should, for instance, depend on tumor size, location, patient comorbidities, availability of a technique, institutional and physician expertise, and patient preference.
Looking ahead, randomized controlled trials across larger patient populations are needed to further elucidate the long-term cancer and survival outcomes associated with these ablative treatments. Research comparing ablative methods with surgery and surveillance as well as exploring other relevant clinical outcomes, such as cost-effectiveness and quality of life, should be performed as well.
“Prospective randomized trials remain essential to further refine the position of SBRT in clinical practice in patients who are surgical candidates,” Siva told Medscape Medical News.
This research had no commercial funding. Raman reported receiving personal fees from AstraZeneca, Sanofi, Knight Pharmaceuticals, Verity Pharma, and Tersera, and grants from Knight Therapeutics, AstraZeneca, and Varian. Siva reported financial relationships with AstraZeneca and Telix Pharmaceuticals. Helou and Tang had no relevant disclosures.

 Admin_Adham
Admin_Adham