For the first time, researchers have transplanted gene-edited donor islet cells that secrete insulin in a person with type 1 diabetes (T1D) without the use of immunosuppression.
Twelve-week results from the phase 1, single-participant study were published online on August 4, 2025, as a Brief Report in The New England Journal of Medicine. Six-month data were presented on June 23, 2025, at the American Diabetes Association (ADA) 85th Scientific Sessions in Chicago and announced at the time in a press release from Sana Biotechnology.
The study subject, a 42-year-old man with a 37-year history of T1D, has shown no immune response to the gene-edited cells and has maintained ongoing significant circulating C-peptide levels, a measure of insulin secretion, in contrast to zero at baseline. MRI at 12 weeks confirmed persistence of the grafted hypoimmune islets. At 6 months, increased C-peptide levels in response to a mixed-meal tolerance test were seen.
He still requires insulin treatment, but that was expected because the protocol for this early safety study involved delivery of only 7% of the number of cells that would be curative, lead author Per-Ola Carlsson, MD, PhD, senior physician and professor at the Clinic for Endocrinology and Diabetology at Uppsala University Hospital, Uppsala, Sweden, told Medscape Medical News.
‘Excited,’ but ‘Many Hurdles to Overcome’
Currently, transplantation for treatment of T1D — whether of whole pancreas, cadaveric donor islets, or experimental stem cell-derived islets — is reserved for individuals with frequent severe hypoglycemia or those who are already undergoing another transplant, such as a kidney. In most people with managed T1D, the adverse health risks for immune suppression are viewed as outweighing the benefits of a transplant.
In T1D, transplantation provokes two immune system attacks: one against any foreign body, which is common to all organ transplants (allogeneic), and a second to the beta cell-specific autoantibodies that caused the condition in the first place. Thus far, it appears that this novel gene-editing approach overcomes both allogeneic and autoimmune rejection.
If upcoming trials using stem cell-derived islets that can be produced in unlimited quantities validate these results, this approach could essentially represent a cure for many people T1D, Carlsson said.
“I have never been so excited in my life. I’ve been working with the science since the 1990s, and this is the one project that has been so positive and so convincing. I’m really happy to work with it, and since I’m a clinician, it’s magic to be able to do something that could turn into a reality for these patients,” he told Medscape Medical News.
However, he cautioned, “This is one subject…we believe it is applicable to all subjects with type 1 diabetes. But of course, there may be subgroups that it does not work for.” Moreover, he noted, “It will take time before it reaches clinical reality.”
Experts in the field contacted by Medscape Medical News expressed cautious optimism.
Mark A. Atkinson, PhD, the ADA Eminent Scholar for Diabetes Research and professor in the Department of Pathology at the University of Florida, Gainesville, Florida, said, “I am very enthusiastic about this study. I think this is a baby step, with the potential for moving forward a full leap. Time will tell. At a minimum, this shows that genetic modification of a stem cell source may prove valuable as a future therapeutic for type 1 diabetes.”
However, Atkinson noted that because the treatment is likely to be expensive, “the cost versus benefit ratio of using such a therapy across the spectrum of type 1 diabetes needs further exploration.”
Islet cell transplantation pioneer A.M. James Shapiro, MD, Canada Research Chair in Transplantation Surgery and Regenerative Medicine at the University of Alberta, Edmonton, Alberta, told Medscape Medical News “This is indeed an exciting development in that human insulin-producing islet cells continued to secrete, albeit small amounts of insulin in the absence of immune suppression. Ongoing research will determine whether this approach can be effectively scaled up and engraftment improved.”
David M. Harlan, MD, director of the Breakthrough T1D Barbara D. Cammett Center of Excellence in New England and co-director of the University of Massachusetts (UMass) Diabetes Center of Excellence, Worcester, Massachusetts, said, “I believe that the genetic modifications of stem cell-derived islets and/or a druggable target within a stem cell-derived islet is likely to represent a practical cure for type 1 diabetes in the next decade or so. I’m excited by this step, but I still see many hurdles to overcome.”
Hypoimmune Islets: Breakthrough or Baby Step?
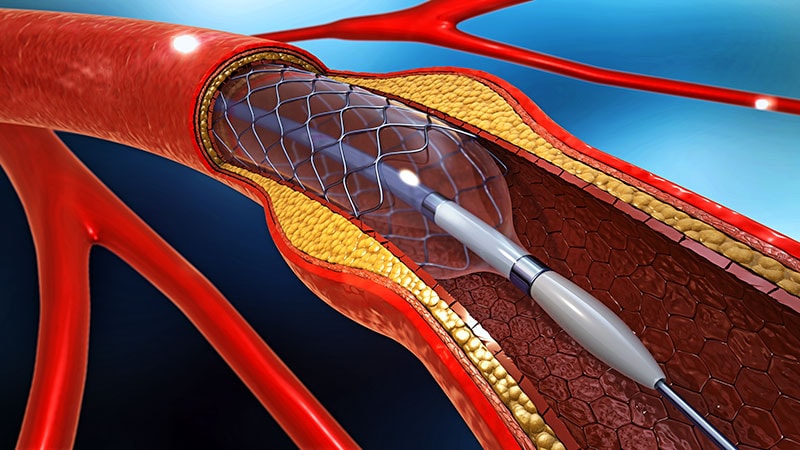
Some of the “hurdles” cited by Harlan, who is also the William and Doris Krupp Professor of Medicine at UMass, relate to the gene-editing procedure itself and to some of the study methodology. The islets, from a deceased donor with the same blood type as the recipient, were first dissociated into single cells, and the genes encoding human leukocyte antigen (HLA) class I and class II were inactivated using clustered regularly interspaced short palindromic repeat. The cells were reclustered, again dissociated, and transduced with a lentiviral vector containing CD47 complementary DNA.
Knocking out HLA class I and II is necessary to protect against adaptive T-cell rejection, while overexpression of CD47 inhibits innate killing via macrophages and natural killer cells, Carlsson explained.
According to Harlan, even without HLA class I and II, there would still be other cell surface molecules that would be expected to provoke an antibody response. “I just don’t understand why they don’t see any donor-specific antibodies against the gene-modified islets. That doesn’t make sense to me. Maybe such antibodies would be benign, but I would still expect them to be picked up.”
Carlsson countered, “Detection of foreign cells is through HLA. Other antigens…are, even if not encoded from the HLA class I or class II genes, presented to the immune system by the HLA molecules.”
Atkinson noted that the autoimmune response could take much longer to occur than the allogeneic, and therefore longer follow-up is needed. Carlsson said that the planned follow-up is 15 years, but prior data suggest that the autoimmunity would occur within 1-2 months, and “we didn’t see any attack at all.”
Harlan also noted that the patient’s high baseline A1c, 10.9%, was unusual and might have adversely affected the findings. Carlsson said that this was per request of the regulatory bodies because such an individual would “gain most from the development of a curing therapy considering their high risk of complications.” He added that this requirement “complicated the study since high glucose stresses the beta cells…we were, however, able to improve his metabolic control post-transplantation.”
The gene-edited cells were delivered with 17 separate injections — to allow for sufficient oxygen exposure — into the patient’s forearm while he was under general anesthesia. Both Harlan and Atkinson questioned the feasibility of that approach going forward. Carlsson said that the forearm was chosen because it was simpler to monitor for safety, but that in future studies abdominal muscles might be used.
Sana Biotechnology will not study this product, UP421, further. Instead, they are moving forward with SC451, a stem cell-derived pancreatic gene-edited islet cell product. The next study is still being planned but will involve multiple patients at more than one clinical site, Carlsson told Medscape Medical News.
Atkinson commented, “Over 50 years ago, individuals with type 1 diabetes were told that a cure was on the way, and it was going to occur through islet cell transplantation and understanding of the autoimmune nature of type 1 diabetes. There were animal models of the disease, and there were new classes of drugs that came out, namely cyclosporine. So, people had hopes that a cure for type 1 diabetes was 3-5 years away. Now, six decades later, we’re still struggling with that, but there's promise on the horizon.”
Carlsson and Shapiro reported having no disclosures. Atkinson is a consultant for Vertex, Sanofi, Diamyd, Novo Nordisk, and Sernova. Harlan is co-founder and chief scientific officer for Stability Health, LLC; a consultant for CG Scientific, Inc.; and chair of the scientific advisory board for TIXiMED.
Miriam E. Tucker is a freelance journalist based in the Washington, DC, area. She is a regular contributor to Medscape Medical News, with other work appearing in the Washington Post, NPR’s Shots blog, and Diatribe. She is on X @MiriamETucker and BlueSky @miriametucker.bsky.social.

 Admin_Adham
Admin_Adham